Can Stem Cells Treat Type 1 Diabetes? Exploring the Potential for Cellular Regeneration
Stem cell therapy has emerged as a promising area of research for treating Type 1 diabetes, which is characterized by the immune system attacking insulin-producing cells in the pancreas. Several studies, including those from Harvard's Stem Cell Institute, have explored innovative approaches, such as the development of stem cell-derived pancreatic islet cell replacement therapies. Current research shows that stem cells have the potential to treat the damage caused by Type 1 diabetes, offering hope for a more effective treatment (Flynn, 2024).
Recent success stories highlight the possibility of using a patient’s own cells for therapy. For instance, a case in China demonstrated that a woman no longer required insulin 75 days after undergoing a stem cell treatment. This indicates that there may be effective strategies on the horizon that could alleviate some of the burdens of managing Type 1 diabetes by restoring insulin production (Flynn, 2024).
While obstacles still remain in bringing these therapies to the mainstream, advancements in stem cell differentiation and protocols could lead to breakthroughs. With ongoing research and clinical trials, the quest to repair Type 1 diabetes using stem cells could significantly change the lives of those affected by this condition.
Type 1 diabetes is an autoimmune condition characterized by the destruction of insulin-producing β-cells in the pancreas. The following sections elucidate the disease's pathophysiology and the current treatment options alongside their limitations (Mayo Clinic, 2024).
In type 1 diabetes, the immune system erroneously targets and destroys β-cells. These cells are responsible for producing insulin, which regulates blood glucose levels. The destruction leads to insulin deficiency, resulting in hyperglycemia (Hackett et al., 2021).

Source: Medium
Key factors include:
The precise cause remains elusive, which complicates finding a definitive cure. Ongoing research aims to understand these mechanisms better.
Current management of type 1 diabetes primarily involves insulin therapy, which can be delivered via injections or insulin pumps. This treatment regimen helps control blood sugar levels but does not restore normal pancreatic function.
Limitations of stem cells to treat diabetes include:
Researchers continue to explore alternatives, including stem cell therapy, which shows potential for restoring insulin production and possibly providing a cure in the future (Delaune, 2024).
Stem cell research presents promising and new avenues for the treatment of type 1 diabetes by addressing the loss of insulin-producing β-cells. Advances in differentiation techniques and clinical trials indicate significant progress in potentially curing this autoimmune condition.
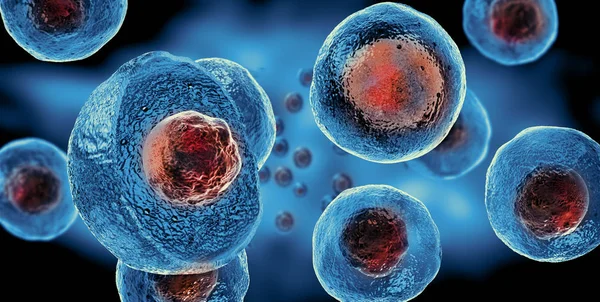
Stem cells, especially pluripotent stem cells, have the potential to differentiate into insulin-producing β-cells. This ability offers the prospect of regenerating the pancreatic cells that are destroyed in type 1 diabetes.

Source: IJMS
Several protocols have been developed to convert stem cells into β-cells, which could restore natural insulin production. The goal is to enable the body to regulate blood glucose levels effectively without exogenous insulin.
Research highlights the potential of generating glucose-responsive cells that secrete C-peptide, an indicator of insulin production. This development raises the question: can type 1 diabetes be cured? While results are promising, consistent long-term outcomes are necessary to confirm success.
Recent clinical trials mark significant milestones in stem cell therapy for type 1 diabetes. An important phase 1 trial involved the transplantation of islets derived from chemically induced pluripotent stem cells. The results showed that a 25-year-old patient maintained insulin independence beyond 75 days post-surgery.
Moreover, ongoing studies are focused on refining transplantation techniques and enhancing the survival of implanted cells. The continuous evolution of these methods suggests that researchers are making strides toward developing viable and effective stem cell treatments for type 1 diabetes in future.
Though a definitive cure for type 1 diabetes through stem cells is not yet realized, the field is advancing. The combination of scientific insights and patient outcomes points toward a hopeful future in diabetes therapy.
The implementation of stem cell therapy for type 1 diabetes raises important considerations regarding accessibility, costs, and regional practices. Understanding these factors can help patients make informed decisions.
The cost of stem cell treatment for type 1 diabetes can vary widely. This discrepancy is dependent on the type of treatment, the facility providing the therapy, and the specific protocols used.

Source: Medical Xpress
Many patients struggle with the affordability of such treatments, especially if not covered by insurance. In some regions, clinical trials may offer reduced costs or even free access for participants.
Patients also need to consider the accessibility of healthcare facilities that provide these therapies. Availability may be limited in certain areas, leading individuals to travel considerable distances, raising additional financial and logistical barriers.
In countries like China, stem cell treatments have been explored with varying methodologies, including the use of a patient’s own cells. Some reports indicate success in patients no longer needing insulin post-treatment.
However, the regulatory environment in China differs significantly from that in the United States and Europe, impacting treatment protocols and patient safety practices.
While some regions may show promising outcomes, the lack of standardized practices can lead to inconsistencies in the quality of care provided. Prospective patients should conduct thorough research on the treatment facilities available in their area.
Shiney Wellness stands out as the no. 1 stem cell therapy center, committed to offering innovative treatments that harness the body's natural healing potential. With a team of highly skilled medical professionals, Shiney Wellness provides personalized care in a state-of-the-art facility. They specialize in regenerative therapies designed to alleviate pain, support recovery, and improve quality of life. By using cutting-edge technology and adhering to the highest standards of safety, Shiney Wellness ensures optimal results for patients seeking alternative solutions for chronic conditions. Trust Shiney Wellness as your partner in achieving enhanced wellness through stem cell therapy.
Delaune. “Intraportal islet transplantation: the impact of the liver microenvironment.” Transplant Int., Stem Cell Research & Therapy, 29 January 2024, https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03636-0. Accessed 02 December 2024.
Flynn, Hannah. “Stem-cell therapy reverses type 1 diabetes in groundbreaking case study.” Medical News Today, Medical News Today, 4 October 2024, https://www.medicalnewstoday.com/articles/stem-cell-therapy-reverses-type-1-diabetes-in-groundbreaking-case-study. Accessed 02 December 2024.
Hackett, Elizabeth, et al. “Type 1 Diabetes: Pathophysiology and Diagnosis.” Pharmaceutical Journal, Pharmaceutical Journal, 2021, https://pharmaceutical-journal.com/article/ld/type-1-diabetes-pathophysiology-and-diagnosis. Accessed 02 December 2024.
Mayo Clinic. “Type 1 diabetes - Symptoms and causes.” Mayo Clinic, 27 March 2024, https://www.mayoclinic.org/diseases-conditions/type-1-diabetes/symptoms-causes/syc-20353011. Accessed 2 December 2024.

